In this blog article, antenatal and newborn screening coordinator Louise Frost explains how the creation of an antenatal booking centre (ABC) improved early access and continuity of care for women at Princess Royal University Hospital (PRUH) in south east London.
Louise also submitted this work as a case for shared learning. Providers, commissioners and other stakeholders are all invited to share examples of learning and good practice relating to NHS population screening programmes.

Background
All pregnant women must be offered sickle cell and thalassaemia screening in pregnancy.
Ideally the result should be available by 10+0 weeks of pregnancy. This target is a key performance indicator (KPI) with an acceptable level of 50% and an achievable level of 75%.
We know many maternity units find meeting these thresholds challenging. This article explains how we went about improving performance and the quality of service women experience at PRUH.
ABC implementation
PRUH has 3 community sites where we offer screening and take blood samples at the first midwife appointment.
In the past we sent referrals to each site to organise women's first midwife appointment separately. In May 2015 we implemented the ABC approach at PRUH and centralised the referral process.
Implementing this approach included:
- triaging all referrals by a midwife to make sure the scan appointment is arranged at the right time
- a dedicated ABC phoneline for women to contact
- updates to the hospital website with links to the Screening tests for you and your baby booklet and its translated versions
- involvement of the maternity services liaison committee which designed a self-referral booking form
- both GP and self-referral forms being made available online
- maintenance of a robust referral database to review services
- directing women to the ABC to self-refer following a confirmed pregnancy within the radiology department (reducing delays)
- ABC staff phoning women to arrange their appointments and reduce the chance of DNAs
- awareness raising among primary care through a GP event and a GP newsletter article
ABC appointment pathway
We aim to offer women a midwife appointment at 9+0 weeks of pregnancy. If this is not possible then an appointment is offered at 12+0 weeks and we invite them to attend a walk-in booking blood clinic before 10+0 weeks.
Post-implementation
Since implementing we have further developed the service by including:
- additional overflow midwife clinics, including at weekends to improve availability
- text message appointment alerts to reduce the number of women not attending
- referral data audit and community team service redesign to reflect findings and ensure continuity of care
- changing the online self-referral form to an automatic submission from the website into the ABC generic email account – the referrals are processed from here
- daily review of appointment waiting times
KPI data for ST2 (timeliness of test) for Princess Royal University Hospital
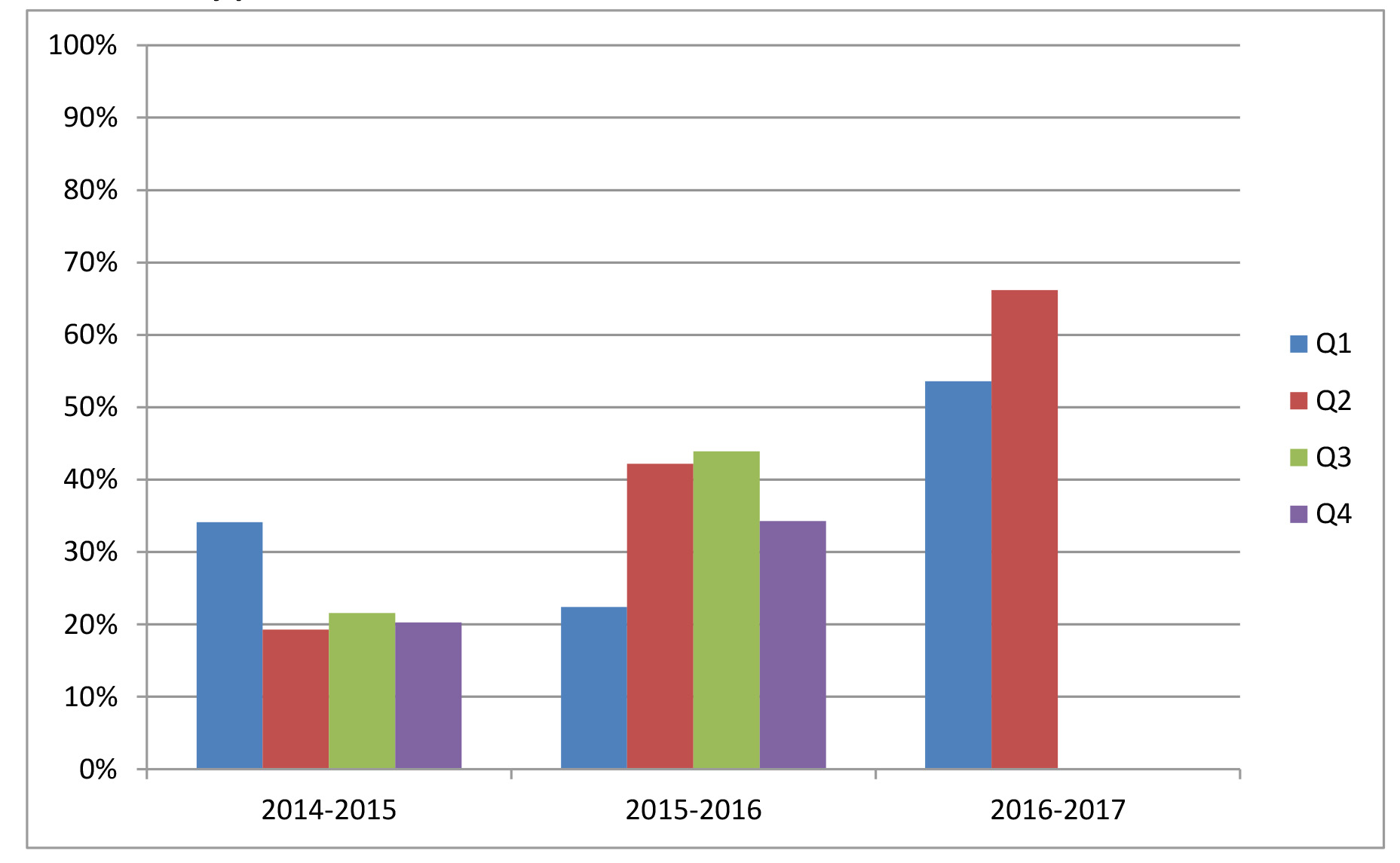
The above chart shows the improvement in performance since the introduction of the ABC approach.
There were no cost implications in setting up this service, which has improved early access and continuity of care for all women.
This service redesign and achievement in improving KPI performance has been recognised by being shortlisted for the Royal College of Midwives Policy into Practice Award.
PHE Screening blog
PHE Screening BLOG articles provide up to date news from all NHS screening programmes – replacing our previously published newsletters.
You can register to receive updates direct to your inbox, so there’s no need to keep checking for new blog articles.
1 comment
Comment by Siobhan Ryan posted on
Well done Louise, really effective initiative