
Sunday 1 December was World AIDS Day. It was an opportunity to reflect on how far we have come in the fight against HIV and AIDS. It was also a time to see how screening in pregnancy for infectious diseases is contributing to improved health outcomes for both women and their babies.
In 2018, Public Health England (PHE) reported 4,453 new diagnosis of HIV in the UK; 26% of these were in women, with just over three quarters being of potential childbearing age.
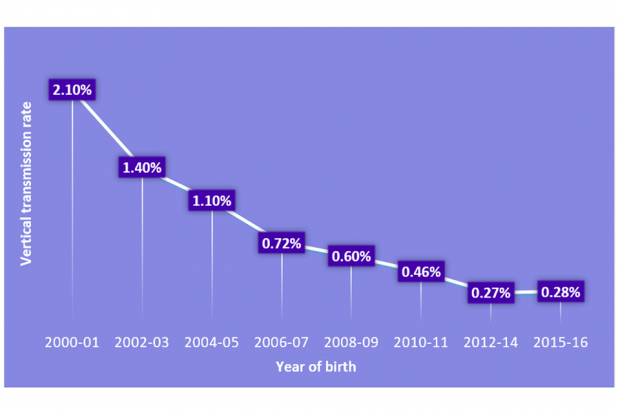
The vertical transmission rate in the UK and Ireland has remained under 0.3% since 2012 (see figure 1).
It reflects the huge success of the antenatal screening programme, clinical care, treatments and interventions in line with the British HIV Association (BHIVA) and the Children’s HIV Association (CHIVA) guidelines.
Figure 1: Vertical transmission rates of HIV among diagnosed women 2000-16 (National Surveillance of HIV in Pregnancy and Childhood)
Higher numbers, more women screened
Uptake of screening for HIV in pregnancy (as a part of the infectious diseases in pregnancy screening (IDPS) screening programme) remains high. The data shows that 99.6% of the almost 660,000 eligible women accepted screening in 2017 to 2018.
Approximately 4,000 women will have a screen positive result each year for HIV, hepatitis B or syphilis, or will be identified as having a prior diagnosis of HIV or hepatitis B. Some women will be identified as having a coinfection with more than one of the infections.
The importance of screening in pregnancy
Screening in pregnancy enables early detection and treatment to significantly reduce the risk of vertical (mother to child) transmission of infection, protecting the health of the woman, her baby and her wider family.
ISOSS has arrived
The IDPS programme Integrated Screening Outcomes Surveillance Service (ISOSS) collects, analyses and reports on a set of important outcomes of the IDPS programme.
The ISOSS team, based at Great Ormond Street’s Institute of Child Health, works with the IDPS programme team at PHE. They are commissioned to carry out the service, building on their experience of running the National Surveillance of HIV in Pregnancy and Childhood (NSHPC), as well as studies commissioned by PHE IDPS programme on HIV, hepatitis B, syphilis and congenital rubella syndrome.
They currently investigate the management of women whose infants acquire HIV vertically to monitor and advise on IDPS programme screening guidance and pathways. The team also work to understand timing and circumstances of how mothers and babies get the infection.
These cases are then taken anonymously to a multidisciplinary expert review panel. Here, they acknowledge common themes, identify likely timings of infection, and discuss missed opportunities.
ISOSS carries out active surveillance of all pregnancies of women living with HIV in the UK, monitoring outcomes of over 1,000 pregnancies per year.
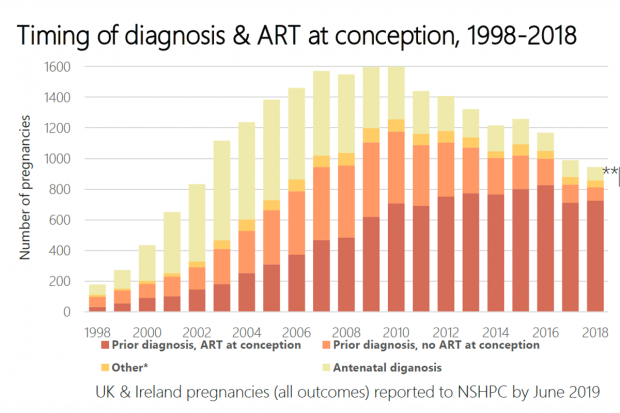
Most women are already aware of their HIV status at booking, and 70% of pregnancies are of women on ART (antiretroviral therapy — the combination of drugs used to treat HIV at conception) (see figure 2). Over 90% of deliveries are to women with an undetectable virus.
Figure 2: Timing of diagnosis and ART at conception, 1998-2018 (National Surveillance of HIV in Pregnancy and Childhood)
Vertical transmissions
Among 25 transmissions reported between 2014 to 2017 (children born 2006 to 2017), 17 were to women undiagnosed at delivery.
As seen in the previous audit, over half of the women experienced difficult social circumstances, uncertain immigration status, intimate partner violence and mental health issues.
Women who declined screening was an important finding in the previous audit. This finding resulted in the programme introducing guidance for the formal re-offer of screening to women that initially decline by 20 weeks' gestation.
The previous audit identified ‘decline screening’ as a contributing factor. This finding helped update programme guidance and standards, and supported the introduction of the formal re-offer of screening by a specialist member of the screening team.
The importance of addressing sexual health during pregnancy remains a priority, with 12 of the 25 transmissions being to women who had a negative test at booking. This means that these women were infected with HIV either during pregnancy or postnatally whilst still breastfeeding their baby.
The IDPS programme team are working closely with the National Infection Service (NSI) on the maternity strand of the PHE syphilis action plan. Raising awareness of sexual health, both in health professionals and the public, is a main objective of this work.
The future of ISOSS
The service will be expanded over the next 18 months to include:
- reporting of suspected congenital syphilis cases (dating back to 1 January 2015)
- maternal syphilis cases from 1 April 2020 via the secure online portal
- maternal hepatitis B and linkage to paediatric outcomes from 1 April 2021
More information and updates will be posted via the blog and the ISOSS website.
PHE Screening blogs provide up to date news from all NHS screening programmes. You can register to receive updates direct to your inbox, so there’s no need to keep checking for new blogs. If you have any questions about this blog article, or about population screening in England, please contact the PHE screening helpdesk.