High quality blood samples are important for the combined test for Down’s syndrome, Edwards’ syndrome and Patau’s syndrome and the quadruple test, which only screens for Down's syndrome.
Samples for both the combined and quadruple test should be taken, stored and transported correctly so they reach the laboratory in a state where they can be analysed to give an accurate result.
My name is Carolyn Williams and I am a consultant biochemist working in antenatal screening. In this article I will be discussing national guidance and explaining why we need standard operating procedures between maternity services and screening laboratories.
Taking the sample
Samples for screening should always be taken into a serum tube. If a full blood count (FBC) and a screening sample are both being taken, it is important that the screening sample is drawn before the FBC. This is to prevent the screening sample from becoming contaminated by a chemical in the FBC tube, meaning it cannot be tested.
Storing the sample
Samples become unstable if they are not processed within a certain time. This affects the screening result and can, in some cases, lead to a false higher-chance result. The NHS website has a good explanation of what we mean by higher and lower-chance results.
Once taken, screening blood samples should be sent to either a regional screening laboratory or a local hospital laboratory for initial processing.
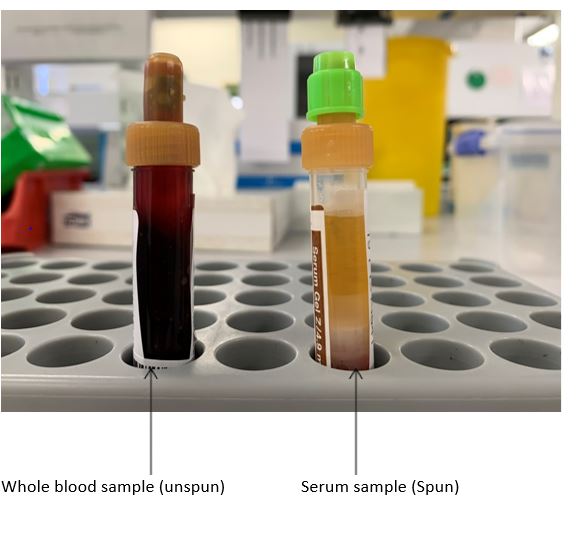
This involves centrifugation (spinning) of the sample to separate the red cells from the serum (the 'water' part of the blood) to make the sample more stable. You can see the difference between a spun and unspun sample in the photo below.
 Temperatures
Temperatures
Screening samples should undergo centrifugation within 48 hours of taking the sample when they are transported and handled at room temperature.
Once centrifuged the serum sample is stable for 72 hours at room temperature.
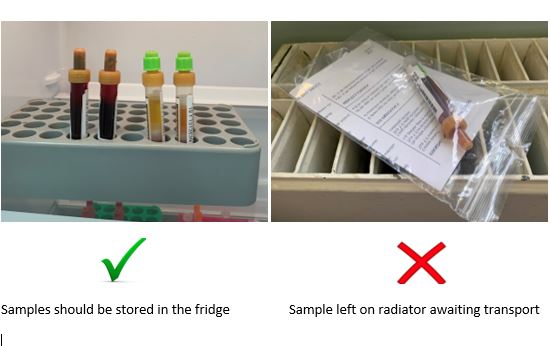
Refrigeration can improve stability greatly. Un-centrifuged samples (whole blood) are stable in the fridge for 5 days and serum samples for 14 days.
Warm temperatures can reduce the stability to only a few hours so care must be taken to keep samples away from radiators and sunny windowsills (see illustration below).
 Transporting the sample
Transporting the sample
Delays in sample transport for longer than 5 days for un-centrifuged samples and 14 days for serum samples can affect the accuracy of the test and lead to potentially misleading results.
Delays in getting the sample to where it needs to be can mean the screening pathway takes longer, as repeat testing is needed.
Therefore, it is important to make sure local sample transport systems fulfil the above criteria so that all women get a valid test result first time.
All samples that are transported or stored at room temperature for longer than 72 hours should be rejected by the screening laboratory.
During transport, samples should ideally be kept cool in cool bags. Whole blood samples should not be frozen or transported on dry ice as this makes them unsuitable for analysis.
Importance of agreed procedures
I'd like to finish off by stressing the importance of having an agreed standard operating procedure between maternity services and screening laboratories (including local laboratories where relevant) about acceptance/rejection of samples.
Crucially, this procedure should meet the above criteria set out in the NHS Fetal Anomaly Screening Programme laboratory handbook.
PHE Screening blog articles provide up to date news from all NHS screening programmes. You can register to receive updates direct to your inbox, so there’s no need to keep checking for new blogs. If you have any questions about this blog article, or about population screening in England, please contact the PHE screening helpdesk.