We, the sickle cell and thalassaemia (SCT) screening programme, recently published a document which defines and clarifies how to determine whether there is a high or low prevalence of SCD and thalassaemia within the area served by an NHS hospital trust. This is vital as it determines which screening algorithm, or model, the trust should use.
We reviewed our recommendations and published this document following enquiries from trusts where high and low prevalence areas were merging and they required advice on which screening algorithm to use.
To establish the prevalence definition for each laboratory, we collated several years’ worth of antenatal data on screen positive women (carriers). This was more fruitful than using the newborn data, as we had done previously to establish the prevalence definition.
The key points from the new publication are detailed below.
There are two different screening algorithms which are used by the SCT programme:
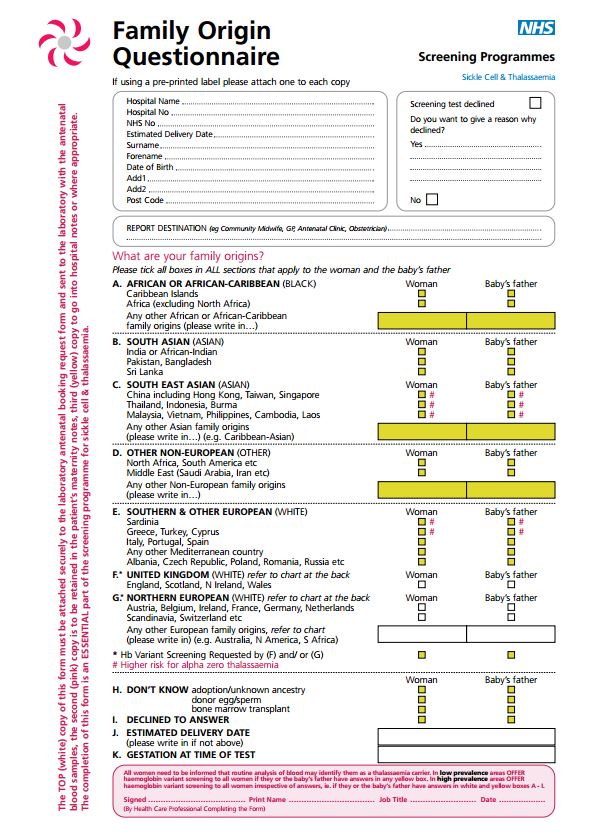
- a family origin questionnaire (FOQ), followed by a blood test for sickle cell and other haemoglobin variants for only those who are deemed at a heightened risk
- screening by a blood test for sickle cell and other haemoglobin variants, and a FOQ
Screening algorithm #1 is used in low prevalence trusts, whereas screening algorithm #2 is used in high prevalence trusts.
When high prevalence and low prevalence trusts merge, it is recommended that low prevalence trusts move to screening algorithm #2, the high prevalence model, as this is regarded as the gold standard.
It is not recommended that high prevalence trusts move to the low prevalence algorithm.
Laboratories should avoid following two algorithms simultaneously - each laboratory should run either the high or the low prevalence algorithm.
PHE Screening blogs
PHE Screening blogs provide up to date news from all NHS screening programmes – replacing our previously published newsletters.
You can register to receive updates direct to your inbox, so there’s no need to keep checking for new blogs.